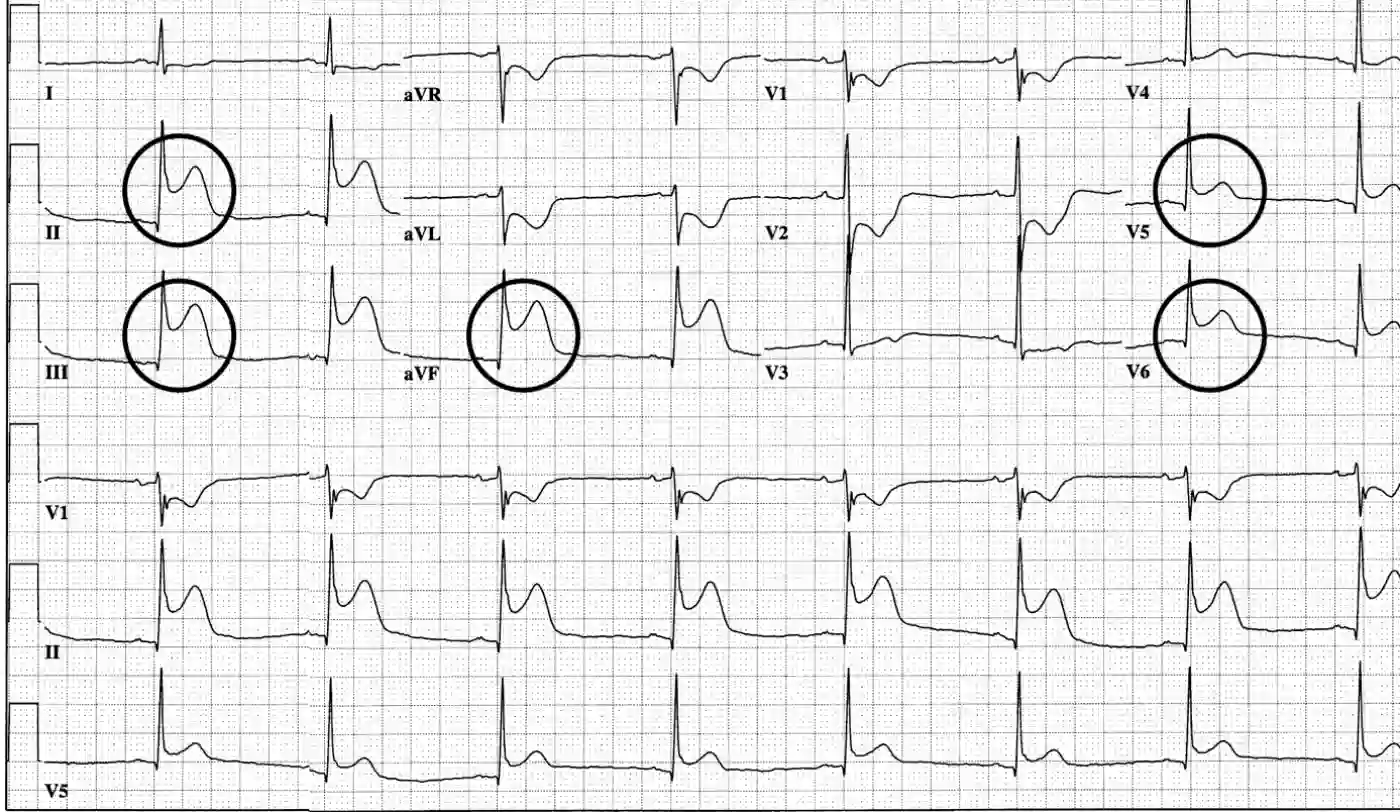
In “inferior t wave abnormality is nonspecific”, we will know how commonly does one encounter Electrocardiograms (ECGs) presenting with subtle deviations? It may involve T waves appearing flat, misshapen, or inverted or even ST segments that are coved, slightly depressed, or indicating J point elevation.
Abbreviated as “nonspecific”, these T waves and ST segment changes in an ECG often do not point clearly toward any specific medical condition. In this context, we delve into potential reasons that may lead to these minor yet irksome changes in ECG, exploring diverse clinical situations where these deviations from normality in T waves and ST segments occur due to the manifestation of an inferior T wave abnormality.
Inferior T Wave Abnormality is Nonspecific: Understanding the Underlying Causes of T Wave and ST Segment Abnormalities
There are circumstances where changes in the T wave might hint at specific conditions, such as the exaggerated T waves in hyperkalemia or symmetrical T wave inversions in the case of myocardial ischemia. But what about other less definitive T wave abnormalities, like flat T waves, biphasic T waves, or asymmetrical T wave inversions?
Additionally, it is possible that ECG ST segment abnormalities stem from a distinct cause, such as myocardial infarction with ST-segment elevation, pericarditis, or myocardial ischemia. At times, the departures from normality might simply be subtle due to an underlying inferior T wave abnormality.
The Role of Inferior T Wave Abnormality is Nonspecific
Thoroughly reviewing ECG findings can help when abnormal ST segment or T wave changes accurately indicate a particular medical condition. Such observations are critical to prevent misinterpretation.
Some conditions like
- Hypokalemia
- Hyperkalemia
- Hypomagnesemia
- Hypermagnesemia
- Hypercalcemia
- Hypocalcemia
- Hyponatremia
They can lead to mild abnormalities, such as slight hyperkalemia or a tiny MI, and may only be indicated by a minor ECG change rather than an outright abnormal finding. An inferior T wave abnormality is nonspecific in such cases, making its understanding vital for the identification of the cause.
Several conditions associated with medication overdoses or cardiac conditions like hypertrophic obstructive cardiomyopathy, Takotsubo cardiomyopathy, Brugada Syndrome, Long QT syndromes, RVH strain, Cocaine toxicity, Loeffler’s endocarditis among others can be associated with an inferior T wave abnormality.
In cases of certain afflictions like Hypothyroidism, Truncal vagotomy, Hypopituitarism, Gallbladder disease, Adrenal insufficiency, Pulmonary embolism, and more, an inferior T wave abnormality could be present.
Every time you come across an ECG with an abnormal T wave or ST segment, employ this list to pinpoint potential causes. There could be other scenarios not listed here; feedback and additional contributions are more than welcome in the comment section.
Unveiling the Link Between Hypertension and Nonspecific ST-T wave Abnormalities: Understanding Inferior T wave Abnormality
Nonspecific changes in ST-segment and T-wave (ST-T) are observed as one of the most frequent electrocardiographic irregularities discovered in patients with hypertension. Nonetheless, only a handful of studies have deliberated on the association of these nonspecific ST-T changes, such as an inferior T wave abnormality, with less than optimum blood pressure (BP) control in hypertensive adults.
And to know if” inferior t wave abnormality is nonspecific”, our study investigated a pool of 15,038 hypertensive patients, selected from a larger group of 20,702 participants from the China Stroke Primary Prevention Trial. The electrocardiogram test conducted at the first visit allowed for monitoring of the baseline heart activity. Based on the test results, the subjects were categorized into two sets: ST-T abnormal and ST-T normal. Inadequate BP control was characterized by systolic BP ≥140 mm Hg or diastolic BP ≥90 mm Hg after hypertensive treatment was administered during a 4.5-year follow-up period. The study employed multivariate analysis to determine the association between nonspecific ST-T abnormalities, like the inferior T wave abnormality, and subpar BP control.
Nonspecific ST-T changes turned out to be rather common in adults suffering from hypertension (approximately 8.5% of the subjects in the study), with a higher prevalence in females (10.3%) and diabetic patients (13.9%). An unsatisfactory BP control rate was reported in a significant portion of the total population (47.0%), especially observable in the ST-T abnormal group (55.5%). The group with nonspecific ST-T abnormalities showed a meaningfully higher chance of unsatisfactory BP control, independent of genetic risk factors. This association was corroborated through the multivariate regression analysis. Noticeable discrepancies were evident among male subjects and individuals with concurrent diabetes.
As a Result
Through this study, we detected increased instances of unsatisfactory BP control in patients with hypertension displaying electrocardiographic nonspecific ST-T changes, notably the inferior T wave abnormality is nonspecific. This was significantly identifiable in sub-categories of male and diabetic patients.
Understanding Primary and Secondary Inferior T Wave Abnormality is Nonspecific

The realm of primary inferior T-wave abnormality is nonspecific, with instances such as ischemia or injury, revolving around amending myocardial cellular electrophysiology. The secondary manifestations like bundle branch block or hypertrophic ventricles, on the other hand, arise due to transforming sequences of ventricular activation.
Dissecting Differential Diagnosis Centered Around T-wave Inversion
Essentially, the 1960s witnessed Jacobson and Schrire outlining the differential diagnosis of T-wave inversion to discover if” inferior t wave abnormality is nonspecific”, reaching onto topics like heart block, ischemic heart disease, bradycardia, right ventricular hypertrophy, right bundle branch block, metabolic and cerebral disturbances. The modern-day differential diagnosis spectrum has broadened to include not just these classical factors, but also complexities like LV anterior wall ischemia, acute nervous system disorders, physiological stress (such as “TTC” Takotsubo cardiomyopathy), pulmonary edema, antiarrhythmic drug effects, pulmonary embolism, cardiac memory linked to transient tachycardia, post-ventricular pacing states, idiopathic causes, and cocaine consumption associated inferences. A recent study demonstrated that 38% of individuals with congenital coronary artery-ventricular multiple micro-fistulas (MMFs) displayed reversible or permanent inverted T-waves, suggesting MMFs’ inclusion in the differential diagnosis of anterior chest wall T-wave inversion.
Exploring Atypical and Persistent inferior t wave abnormality is nonspecific
Certain conditions like acute coronary syndrome, cardiac memory T-wave, non-ischemic cardiogenic pulmonary edema, gastroenteritis, post maxillofacial surgery, subarachnoid hemorrhage, electroconvulsive therapy, Takotsubo cardiomyopathy, pheochromocytoma, and some indeterminate origins can lead to transient T-wave inversions. Contrastingly, enduring T-wave inversion can accompany disorders related to LV or RV cardiomyopathy, comprising apical hypertrophic cardiomyopathy (AHCM) and arrhythmogenic right ventricular cardiomyopathy/dysplasia.
inferior t wave abnormality is nonspecific: Non-coronary Heart and Non-heart Related Disorders
Frequently, non-coronary cardiac and non-cardiac disorders, including pericarditis, myocarditis, cardiac metastasis, athletic heart syndrome, AHCM, hypertrophic cardiomyopathy, post-tachycardia,, and right ventricular pacing, have been found to influence the development of T-wave inversion.
Anticipating Outcomes
As a result of inferior t wave abnormality is nonspecific, among the middle-aged population, an inverted T-wave in the right precordial leads V1-3 usually signals a favorable prognosis. In comparison, inverted T-waves in leads aside from V1-3 are indicative of higher risk outcomes like hospitalization due to congestive heart failure and coronary artery disease. Interestingly, shallow uneven T-waves, with their descending limb more pronounced than the abruptly ascending limb, in middle-aged women do not necessarily denote heart ailments.
Delving into Non-coronary Non-cardiac Disorders
Non-coronary disorders unrelated to the heart could manifest because inferior t wave abnormality is nonspecific and T-wave abnormalities involve severe brain injuries (like subarachnoid hemorrhage and intracranial hemorrhage), traumatic head injuries, maxillofacial surgeries, bilateral carotid endarterectomy, vagotomy aftermath, cocaine abuse, flecainide usage, pheochromocytoma, and gastrointestinal emergencies.
Transient T-wave Inversion Experiences
Symptoms such as T-wave inversion in the precordial leads noticed as far back as 1982, characterized by acute, symmetric, and tight waves typical of the “coronary type”, are usually indicative of substantial stenosis of the proximal left anterior descending coronary artery, contributing to regional ventricular repolarization delay often found in ischemic heart disease. Here, T-wave inversion may prolong for days or weeks.
Memory T Wave History of Inferior T Wave Abnormality is Nonspecific: Cardiac Memory Pattern
In cases featuring intermittent right ventricular pacing, such as presented by Chatterjee and colleagues in 1969, memory T waves were noted in 94% of patients. This pattern – transient T-wave inversion following sinus rhythm restoration after tachycardia or artificial pacing – roots from anomalous ventricular activation. This T-wave inversion pattern in RV pacing owes its existence to discordant LV activation, and the involvement of potassium ion channels is postulated to play an essential role in their pathogenesis. And that is how we find out that inferior t wave abnormality is nonspecific for many logical reasons.
Read more: Panic focused psychodynamic psychotherapy