Coronary artery disease (CAD) is a medical phrase referring to conditions influencing the arteries tasked with delivering nutrients, oxygen, and blood to the heart. Strongly linked with this is the nursing diagnosis for CABG.
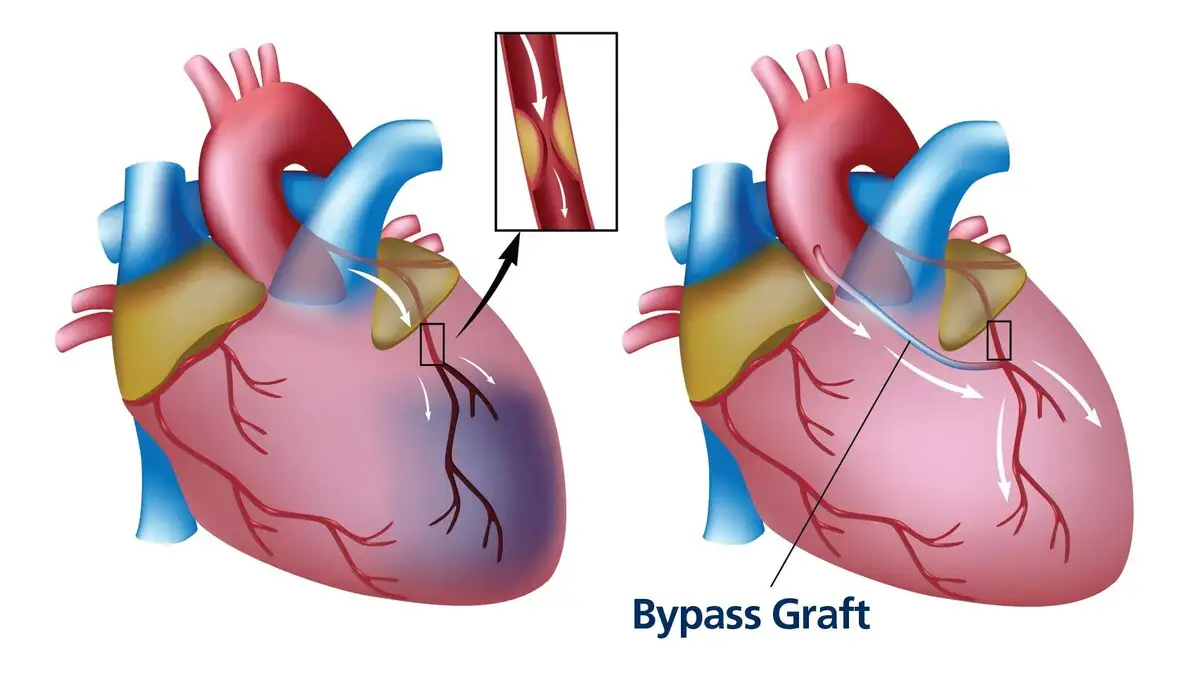
Atherosclerosis, a leading cause of CAD, is typified by the accumulation of lipid deposits within the arterial walls. These disruptive plaques cause arterial narrowing and hinder the smooth flow of blood, thereby heightening the risk of angina and myocardial infarction.
The progression of CAD is a slow, imposing process that spans several years. It’s not uncommon that patients show advanced stages of this condition before they present symptoms such as angina, breathlessness, and exhaustion, hence the key role of the nursing diagnosis for CABG.
In instances where the course of blood through the coronary arteries becomes restrained or fully blocked, ischemia and infarction occur within the heart muscles. The subsequent shortage in blood and oxygen supply (ischemia) to the heart muscle tissue leads to reduced tissue perfusion and death of heart muscle cells (infarction). At this juncture, the nursing diagnosis for CABG is essential as immediate intervention is crucial.
First: Nursing Diagnosis for CABG: An Initial Assessment
The foremost step in nursing care involves an assessment specifically tailored for a nursing diagnosis for coronary artery bypass grafting (CABG). In this phase, nurses compile a comprehensive profile of the patient’s physical health, their emotional state, psychosocial context, and diagnostic data. We delve into both objective and subjective data associated with coronary artery disease for CABG patients.
Subjective Data Analysis
Evaluation of medical history and presenting complaints
1. Enquire about the patient’s general symptoms.
Take into account the patient’s general complaints and symptoms, which might include:
- Chest discomfort
- Shortness of breath (dyspnea), both while resting and during activity
- Rapid breathing (tachypnea)
- Challenges in breathing when lying flat or sitting up (orthopnea)
- Episodes of fainting (syncope)
- Heart palpitations
- Fluid buildup in lower extremities (edema)
- Pain in the lower extremities
- Struggles with physical activities
2. Encourage a precise description of the patient’s chest discomfort.
Request the patient to define the nature of their chest pain, covering aspects like:
- Chest tightness
- Sensation of constriction
- A feeling of heaviness
- Burning sensations
- Pain induced by physical exertion
- Potential triggers such as stress or substance abuse
- Pain emanating towards the jaw, neck, left arm, or back
3. Evaluate the client’s risk factors.
Non-changeable risk elements:
- Age: Aging increases the possibility of damage and narrowing of arteries.
- Gender: Although men are at a higher risk, the risk for women escalates post-menopause.
- Familial history of ischemic heart disease: A significantly high risk exists if a male relative (father or brother) developed heart disease before age 55 or if a female relative (mother or sister) had it before age 65.
- Race/Ethnicity: Certain groups like Hispanics and Blacks show a higher incidence of CAD.
Changeable risk factors:
- Hypertension: If left unchecked, high blood pressure can lead to stiffening of arteries and subsequently reduce the blood flow due to coronary artery narrowing.
- Hyperlipidemia/hypercholesterolemia: An excessive level of “bad” cholesterol (low-density lipoprotein – LDL) or a decrease in “good” cholesterol (high-density lipoprotein – HDL) promotes the onset of atherosclerosis.
- Diabetes or insulin resistance: These conditions can lead to hardening of blood vessels and fatty plaque accumulation.
- Kidney disease: This problem hampers the blood pressure regulation function of the kidneys.
- Tobacco use: Both direct and secondhand smoke elevate the constriction of blood vessels.
- Obesity: It raises cholesterol levels, contributing to arterial plaque buildup and vessel narrowing.
- Physical inactivity: Sedentary behavior escalates cholesterol levels in the blood.
- Diet: Consumption of saturated fat-heavy food can skyrocket LDL “bad” cholesterol.
- Stress: High stress levels result in an increase of inflammatory levels, leading to the constriction of blood vessels.
- Alcohol use: Overuse of alcohol weakens heart muscles and impacts blood clot formation, thus obstructing blood vessels.
- Poor sleep: Insomnia and irregular sleep habits amplify stress levels, leading to blood vessel constriction.
4. Inspect the patient’s past treatments and medication history.
Certain medications (e.g., anthracyclines, anabolic steroids) and past vascular surgeries can compromise the structural integrity of blood vessels.
Second: Objective Data Gathering for a Nursing Diagnosis for CABG
Comprehensive Physical Assessment
we’ll delve into some ways you can gather data for a nursing diagnosis CABG
1. Keep track of vital signs.
Given the diminished supply of oxygenated blood to the heart, significant changes or escalations, particularly in pulse rate and blood pressure, are anticipated in the context of a nursing diagnosis for CABG.
2. Implement EKG and telemetry monitoring.
Prompt action should be taken to carry out an EKG as soon as a patient exhibits symptoms of chest pain in order to check for dysrhythmias. Continuous telemetry monitoring is highly recommended for patients with established cardiac histories.
3. Adopt a systematic assessment framework:
- Neck: Look for signs of distended jugular veins.
- CNS: Monitor for acute distress, dizziness, faintness, fainting, and fatigue.
- Cardiovascular: Be aware of rapid heartbeat, chest discomfort, unusual heart sounds like murmur at the apex or bruit on the carotid artery through auscultation, and irregular heartbeats or arrhythmias.
- Circulatory: Look for reduced peripheral pulses.
- Respiratory: Watch out for signs of shortness of breath, rapid breathing, difficulties breathing when sitting or lying down, unusual sounds like crackles upon auscultating, and intolerance to activities.
- Gastrointestinal: Be aware of symptoms like nausea and vomiting.
- Lymphatic: Monitor for peripheral swelling or edema.
- Musculoskeletal: Check for pain in the neck, arm, back, jaw, and upper body, as well as manifestations of fatigue.
- Integumentary: Look out for skin pallor, cyanosis, and excessive sweating.
4. Determine the patient’s risk.
Compute the patient’s ASCVD (atherosclerotic cardiovascular disease) risk score in the frame of nursing diagnosis for CABG. A lower score (below 5%) is ideal. This provides an objective measure of the patient’s 10-year risk of CAD and other heart diseases, incorporating considerations such as:
- Age
- Gender
- Race
- Blood pressure
- Cholesterol levels
- Medication history
- Diabetes presence
- Smoking prevalence
Third: Establishing a Nursing Diagnosis for CABG with Diagnostic Procedures
1. Evaluate for Arrhythmias.
The genesis of coronary artery disease (CAD), often leading to a nursing diagnosis for CABG, lies in the accumulation of fatty deposits which narrow the heart vessels, impeding blood flow. This constriction often results in a disturbance of the heart’s electrical activity, manifesting as arrhythmias. Keep an eye out for any variances in the ST segment that potentially suggest cardiac ischemia. Be aware of the possibility of other arrhythmia conditions such as atrial fibrillation, bundle branch block, and supraventricular tachycardia.
2. Procure Samples for Laboratory Tests.
Crucial to the nursing diagnosis for CABG is the examination of several laboratory test results:
The Complete Blood Count (CBC) with differential may reveal an underlying infection (indicated by WBC), blood’s clotting ability (platelets), and markers of anemia (from reduced RBC levels).
B-type Natriuretic Peptides (BNP) indicate a possible volume overload of cardiogenic origin. These readings can be misleadingly high due to kidney conditions or low in cases of obesity.
Cardiac enzymes, like Troponin and CK levels, provide valuable indicators of acute ischemia.
Lipid panel tests assist in tracking hypercholesterolemia.
Ultra-sensitive C-reactive protein (us-CRP) or high-sensitivity CRP is a measure of vascular inflammation, a factor elevating the risk of developing CAD.
Liver function tests (LFT) serve to assess the condition of both heart and liver concurrently, as seen in hemochromatosis (a CAD complication caused by excessive iron accumulation in the body). It’s also crucial to monitor liver function, given how it can be affected by cholesterol medication.
3. Facilitate a stress test for the patient.
Stress testing is an effective, non-invasive method to evaluate CAD and plays a significant role in the nursing diagnosis for CABG. It provides valuable insight into the heart’s response to physical exertion.
4. Prepare the patient for Cardiac Catheterization.
Regarded as the most accurate and reliable technique for observing the heart’s vessels, cardiac catheterization (or angiogram) carries inherent risks due to its invasive nature and the use of contrast dye.
5. Conduct Additional Investigations.
Further procedures can provide more insight for a comprehensive nursing diagnosis for CABG:
The Echocardiogram can reveal structural defects and valve functionality of the heart, aiding in diagnosing valve abnormalities or underlying conditions such as heart failure.
Perform an Exercise Treadmill Test on patients with a normal resting ECG and capable of physical exercise.
The Nuclear Stress Test, a complement to the exercise stress test, merges ECG readings with images depicting blood flow to the heart, both at rest and under stress.
Stress imaging is recommended for patients who have already undergone revascularization, those with difficult-to-interpret ECGs, or patients with physical constraints that restrict exercise.
Cardiac CT scans are instrumental in identifying calcium deposition and blockages in the heart’s arteries.
A CT Coronary Angiogram, similar to a cardiac CT scan but using contrast dye, furnishes a more in-depth image.